Research Topics
Sickle cell disease (SCD) has its roots in genetic mutations that cause a single amino acid change in the β-globin chain of hemoglobin A and thereby confer protection against malaria. Whereas one copy of the mutated gene is an asset in areas where malaria is endemic, two copies become a liability regardless of geographic location. The unadulterated mutation encourages hemoglobin to clump and deform red blood cells, leading to anemia, increased hemolysis, and vascular occlusions that affect multiple organs. Dr. Tisdale is working on multiple strategies both in the laboratory and in the clinic to cure sickle cell disease by repairing or replacing the precursor bone marrow cells that give rise to sickled red blood cells.
Bone marrow transplants from healthy donors are used successfully to treat certain blood cancers for which the course of the disease is so severe that the destruction of the patient’s own immune system through high-dose chemotherapy and radiation seems an effective compromise. However, the therapeutic balance in the case of SCD is less clear; children tolerate transplants more successfully, but they are also less imminently threatened by the disease. The success of conventional transplants in adults, whose need is more immediate, is less clear.
The issue of immune tolerance is, of course, central to transplantation research. Dr. Tisdale has an active research program in trying to characterize tolerance and create conditions in which patients will more easily tolerate donor cells and tissues without the need for destroying the immune system or perpetual use of immunosuppressant drugs.
Dr. Tisdale and his colleagues recently completed a modified bone marrow transplant strategy for the first time in adult patients with sickle cell disease. In a recent study, they demonstrated that they could transplant bone marrow cells from HLA-matched sibling donors without needing to completely destroy the patient’s immune system. This “mixed chimerism” appears to persist without the need for the ongoing immunosuppression that other types of transplants require. The important innovation in the protocol was the short-term destruction of the patient’s T-lymphocytes through a depleting antibody, followed by their regrowth under the influence of the mTOR inhibitor rapamycin. The next phase of this work is to extend the concept with alternative strategies to include donors who are not perfectly matched (thereby including a half-matched sibling, parent, or child).
Dr. Tisdale and his colleagues also have an ongoing research agenda to find a gene therapy strategy for SCD. After extracting and isolating precursor CD34+ cells from patients, they use viral transduction to insert a correct copy of the β-globin gene before returning the cells to the patient’s bone marrow. The laboratory has focused on optimizing the conditions for viral transduction, including selecting and modifying viral strains for study in animal models, optimizing growth conditions for transduced hematopoietic cells, and designing gene vectors to ensure appropriate placement and expression of the inserted gene.
Finally, strategies to correct the underlying mutation which causes SCD are being pursued utilizing newly developed gene editing tools, and work in the laboratory to develop methods for efficient editing of hematopoietic stem cells is underway.
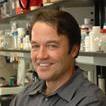
Biography
John Tisdale, MD, is a senior investigator and chief of the Cellular and Molecular Therapeutics Branch of the National Heart, Lung, and Blood Institute (NHLBI) at NIH. Dr. Tisdale’s research focuses on developing curative strategies for sickle cell disease through transplantation of allogeneic or genetically modified autologous hematopoietic stem cells. He received his medical degree from the Medical University of South Carolina (MUSC) and trained in internal medicine at Vanderbilt University, where he also completed a chief residency. After a postdoctoral fellowship in NHLBI’s Hematology Branch, he joined the Molecular and Clinical Hematology Branch of NHLBI in 1998.
An elected member to the American Society for Clinical Investigation, Dr. Tisdale is the recipient of the Ernest Beutler Lecture and Prize of the American Society of Hematology. His awards include the American Society of Gene and Cell Therapy’s Jerry Mendell Award for Translational Science, the George C. Marshall Innovation Leadership Award, the Public Health Service Outstanding Service Medal, the Annual Bipartisan Congressional Silver Innovator Award, the American College of Physicians’ Richard and Hinda Rosenthal Award #1, and the College of Charleston’s Pre-Medical Society’s Outstanding Service Award in Medicine. He was a finalist of the Samuel J. Heyman Service to America Medal and is one of four clinicians featured in Discovery Channel’s “First in Human” documentary on clinical trials conducted at NIH.
Dr. Tisdale has over 250 publications. He was the Principal Investigator on the gene therapy trial of lovo-cel for SCD that was FDA approved in 2023.
Selected Publications
- Kanter J, Walters MC, Krishnamurti L, Mapara MY, Kwiatkowski JL, Rifkin-Zenenberg S, Aygun B, Kasow KA, Pierciey FJ Jr, Bonner M, Miller A, Zhang X, Lynch J, Kim D, Ribeil JA, Asmal M, Goyal S, Thompson AA, Tisdale JF. Biologic and Clinical Efficacy of LentiGlobin for Sickle Cell Disease. N Engl J Med. 2022;386(7):617-628.
- Hsieh MM, Fitzhugh CD, Weitzel RP, Link ME, Coles WA, Zhao X, Rodgers GP, Powell JD, Tisdale JF. Nonmyeloablative HLA-matched sibling allogeneic hematopoietic stem cell transplantation for severe sickle cell phenotype. JAMA. 2014;312(1):48-56.
- Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R, Childs RW, Rodgers GP, Powell JD, Tisdale JF. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009;361(24):2309-17.
- Demirci S, Zeng J, Wu Y, Uchida N, Shen AH, Pellin D, Gamer J, Yapundich M, Drysdale C, Bonanno J, Bonifacino AC, Krouse AE, Linde NS, Engels T, Donahue RE, Haro-Mora JJ, Leonard A, Nassehi T, Luk K, Porter SN, Lazzarotto CR, Tsai SQ, Weiss MJ, Pruett-Miller SM, Wolfe SA, Bauer DE, Tisdale JF. BCL11A enhancer-edited hematopoietic stem cells persist in rhesus monkeys without toxicity. J Clin Invest. 2020;130(12):6677-6687.
- Fitzhugh CD, Cordes S, Taylor T, Coles W, Roskom K, Link M, Hsieh MM, Tisdale JF. At least 20% donor myeloid chimerism is necessary to reverse the sickle phenotype after allogeneic HSCT. Blood. 2017;130(17):1946-1948.
Related Scientific Focus Areas
This page was last updated on Thursday, August 21, 2025